Billions of people use social media every day. This has changed the way we communicate with each other. These days, the average user spends 2 hours and 16 minutes every day on social media platforms. Although social media has given us an open door to more information than ever before, there are good and bad effects on our mental health due to our use of this technology.
What Is Social Media?
In simple words, social media is a computer-based technology that facilitates sharing your ideas, thoughts, and information. This is done through the building of virtual networks and communities. People engage with social media through a computer, tablet, or smartphone by using web-based applications.
What Is Social Media’s Effect on Mental Health?
 There has been substantial growth in the use of social media in recent years. The Pew Research Center found that 72% of Americans in the U.S. use social media. However, since social media use is still relatively new, there aren’t any long-term studies recording the effects of social media.
There has been substantial growth in the use of social media in recent years. The Pew Research Center found that 72% of Americans in the U.S. use social media. However, since social media use is still relatively new, there aren’t any long-term studies recording the effects of social media.
Still, several recent studies show that social media impacts mental health in several ways. As a result, the increasing dependence on the use of social media puts a large number of Americans at an increased risk for feeling:
What Are The Positive And Negative Effects Of Social Media?
Positive: Increases our awareness
One of the great benefits of social media is that a person or organization can quickly increase awareness of an important issue to a huge audience. More people are using social media every day to promote change and help make positive changes in the world.
Negative: May contribute to fake news.
Even though many social media platforms have taken steps to try to combat fake news, it hasn’t stopped the worldwide spread of misinformation. Anyone with a computer or smartphone can share information with a massive audience and when used with bad intentions, it can have bad results.
Positive: It can help combat loneliness
Humans are social creatures with a need to socialize and connect with other people. Frequently, social media is blamed for replacing face-to-face communication. However, for some, social media is a way to promote conversations with like-minded people and build friendships. A recent survey showed that 70% of senior citizens are using social media to stay in touch with family, friends, and the outside world.
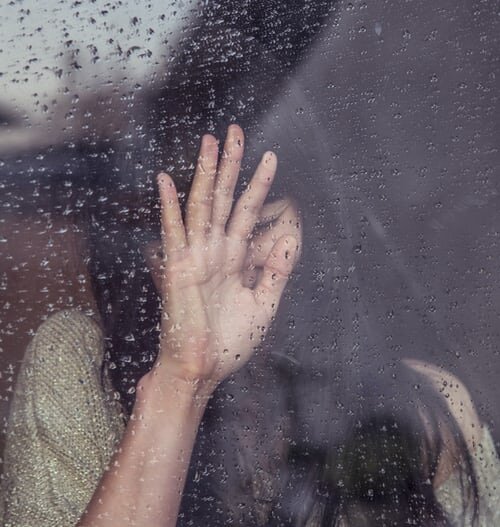
Negative: It can increase the feelings of loneliness and isolation
According to something called “social displacement theory,” the more time people spend on social media, the less time they are likely to spend face-to-face socializing. Although social media was meant to increase social interactions, a survey found that those people who spent more time on social media every day felt lonelier than people who checked their social media less. Despite social media bringing people together digitally, it could be risking our in-person relationships and increase feelings of disconnection and isolation.
Positive: It makes you feel like you are not alone and part of a community
It’s very typical to feel hesitant about talking to family and friends about health issues. But with so many health services and information available online, social media can give a person a safe space to ask questions and connect to a slew of health resources. For people living in a remote or rural area, social media is an inexpensive and usable option for getting help by providing resources to people who may not have access any other way.
Negative: It may support antisocial behavior
When it’s not used properly, social media can have unhealthy consequences for your mental health. If social media takes the place of any face-to-face interactions, it increases the likelihood of antisocial behavior. Although meant to bring us together, when social media is used incorrectly it can lead us to compare our lives with other peoples’ and have a hurtful impact on our well-being. Social media tends to only show the best parts of someone’s life. So, if you spend too much time looking at misleading or biased content, it can make you feel deficient in some way and cause serious psychological and physical problems including self-esteem.
Positive: It creates and maintains relationships
Because social media has changed the way we communicate with each other, it has changed how we make and preserve relationships. It is not only a useful tool for individuals who are looking for other people who share their views and have similar interests. It also provides an opportunity to meet and stay in touch with people from all over the world.
Negative: Cyberbullying
Even though social media creates opportunities to meet like-minded people and can help to support positive relationships and discussions, cyberbullying and trolling are major contributors to feelings of anxiety and depression. Cyberbullying is the use of technology to harass, bully, and intimidate another person. A recent study discovered that cyberbullying is associated with depression and suicide among teenagers. Furthermore, reports are suggesting that cyberbullying is increasing. Sadly, it’s an ongoing issue that is difficult for social media platforms to reduce.
 Signs That Social Media Is Affecting Your Mental Health
Signs That Social Media Is Affecting Your Mental Health
- It distracts you from work or homework.
- You use it to escape from negative emotions.
- You’re being cyberbullied or trolled.
- You spend more time online than with your family and friends.
- Your feelings of anxiety, depression, and loneliness are increasing sharply.
Social Media and Depression in Teens
The new research analyzed several studies of cyberbullying on social media and found that it is associated with depression in teenagers. Young people being victimized online has gotten a lot of attention, particularly after a series of suicides of teenagers who were bullied on various social networks.
The use of social media is common with teenagers, but the health effects of cyberbullying are mainly unknown. Regular, in-person bullying during the teen years may double the risk of depression in adulthood and the effects of bullying can be as bad as or worse than child abuse.
6 Tips To Protect Your Mental Health From Negative Effects Of Social Media
According to the American Psychiatric Association, more than one-third of adults in America believe social media is harmful to their mental health. And only 5% see it as being positive. Another 45% say it has both negative and positive effects. So here are 6 tips for protecting your mental health:
- Set a limit for when and where you use social media: You’ll have better connections with the people in your life if you set certain times each day when your notifications are off or your phone is in airplane mode.
- Have detox periods: Plan for regular multi-day breaks from social media. Several studies show that even a 5-day break from Facebook can lower your stress and improve your satisfaction with life. And you don’t have to go cold turkey. Just cutting back can result in lower loneliness and depression.
- Pay attention to what you do and how it makes you feel: Try using your favorite platforms for different amounts of time and at different times of the day. You may feel better after a few short spurts online than after 45 minutes or more.
- Use social media mindfully: Ask yourself why you’re using it. Are you trying to avoid something?
- Unfollow those who don’t serve a purpose: Take time to unfollow contacts or groups that are annoying or worse. Most won’t notice and your life will be better for it.
- Don’t let social media fool you, it’s not always realistic: Remember, most people post only what they want you to see on social media. Using platforms such as Facebook to keep up with friends and relatives is fine, but don’t let it be a replacement for in-person interactions.
Live Life, Don’t Just Read About It
Are you dealing with the negative effects of social media? Or are you dealing with depression and don’t know why? You know when you aren’t feeling quite right, whether it’s a result of social media or not. At Lido Wellness Center, we can work through this together and get you back to a more fulfilling life.
Sometimes having a pre-existing mental condition can lead to substance abuse as a means to cope. At Lido Wellness Center, if you have developed multiple conditions, our dual diagnosis program can help treat your co-occurring disorder.
Let us help you improve the way you feel and experience greater mental and emotional well-being. Contact us today.
References
www.ontheline.org.au
www.livescience.com
www.investopedia.com
www.theconversation.com


 There has been substantial growth in the use of social media in recent years. The Pew Research Center found that 72% of Americans in the U.S. use social media. However, since social media use is still relatively new, there aren’t any long-term studies recording the effects of social media.
There has been substantial growth in the use of social media in recent years. The Pew Research Center found that 72% of Americans in the U.S. use social media. However, since social media use is still relatively new, there aren’t any long-term studies recording the effects of social media.  Signs That Social Media Is Affecting Your Mental Health
Signs That Social Media Is Affecting Your Mental Health The American Disabilities Act (ADA) has been in place since 1990 to prevent discrimination against individuals with disabilities in the workplace. The ADA classifies a disability as a physical or mental impairment that substantially limits one or more of the major life activities of an individual. This means that any physical or mental condition is protected as a disability if it impacts a person’s capabilities.
The American Disabilities Act (ADA) has been in place since 1990 to prevent discrimination against individuals with disabilities in the workplace. The ADA classifies a disability as a physical or mental impairment that substantially limits one or more of the major life activities of an individual. This means that any physical or mental condition is protected as a disability if it impacts a person’s capabilities. Neurocognitive disorders
Neurocognitive disorders Once enough evidence has been established, you or a loved one have the option to receive social security disability for mental disorders. Social Security Disability Insurance (SSDI) and Supplemental Security Insurance (SSI) provide options for people with disabilities to receive financial assistance. However, SSDI is only available to those who have been able to work in the past and have contributed to Social Security taxes.
Once enough evidence has been established, you or a loved one have the option to receive social security disability for mental disorders. Social Security Disability Insurance (SSDI) and Supplemental Security Insurance (SSI) provide options for people with disabilities to receive financial assistance. However, SSDI is only available to those who have been able to work in the past and have contributed to Social Security taxes.